How many generators does a hospital need?
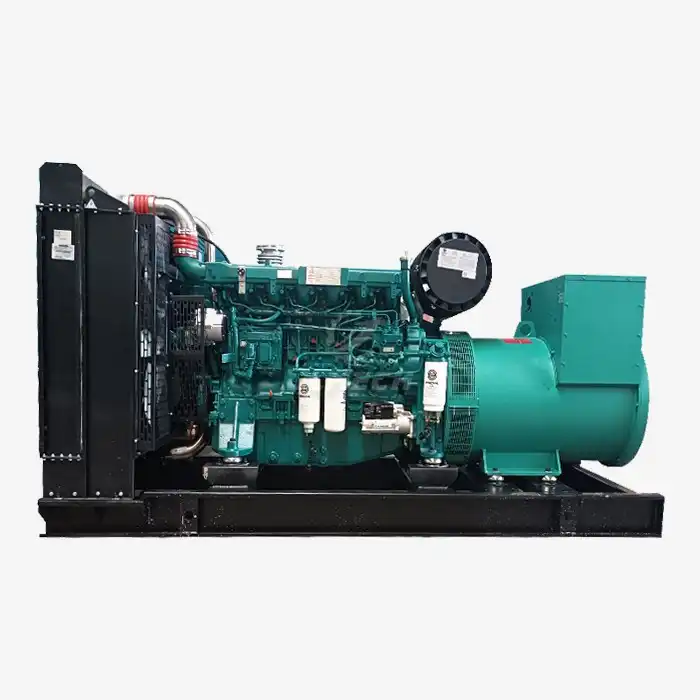
When the power grid fails, hospitals become islands of life-saving activity in a sea of darkness. Unlike any other building type, healthcare facilities cannot afford even momentary power interruptions that could endanger patient lives. Determining the right number of generators for a hospital is not a simple calculation—it's a complex engineering decision that balances regulatory requirements, clinical needs, and operational resilience. Understanding the fundamental hospital backup power requirements is the first step in designing a power system that ensures continuous patient care under any circumstances. This comprehensive guide examines the key factors that determine generator quantity and configuration for healthcare facilities.

Key Determining Factors
The number of generators a hospital needs depends on several interrelated variables. A one-size-fits-all approach doesn't work in healthcare power design, as each facility has unique operational requirements and risk profiles.
Hospital Tier and Size: A community hospital may have different needs than a tertiary care teaching facility with specialized departments like cardiac catheterization labs and advanced surgical suites.
Electrical Load Classification: Hospitals must distinguish between life safety loads, critical loads, and equipment loads, each with different backup requirements . The generator system must accommodate all these classifications according to strict hospital backup power requirements.
Clinical Services Offered: Facilities with trauma centers, neonatal ICUs, and operating rooms require more robust backup systems than those offering primarily outpatient services.
Regulatory Compliance: International standards like Health Technical Memorandum (HTM) 06-01 and local building codes establish minimum requirements that must be met .
Redundancy Needs: For critical care facilities, N+1 redundancy (having one more generator than necessary to handle the load) may be essential to ensure reliability during generator maintenance or unexpected failures.
Hospital Electrical Load Classifications
Hospitals categorize their electrical loads into distinct classes based on criticality to patient safety and operational continuity. This classification system directly impacts generator sizing and quantity.
Life Safety Loads: These include emergency lighting, exit signs, and power for evacuation systems. They represent the absolute minimum load that must be supported.
Critical Loads: This category encompasses patient care areas where power interruption would immediately endanger life . These include:
Intensive Care Units (ICUs) and Critical Care Areas
Operating Rooms and Anesthesia Workrooms
Emergency Departments and Trauma Rooms
Cardiac Monitoring Units and Catheterization Labs
Equipment Loads: These include additional medical equipment and systems that support patient care but may have slightly less stringent backup requirements.
Proper load classification ensures that the most vital functions receive priority during power transitions, directly influencing hospital backup power requirements and generator sizing decisions.
Critical Areas with Special Power Needs
Certain hospital departments have exceptional power reliability needs that often dictate specific generator configurations and supplemental systems.
Surgical Suites: Operating rooms require not only generator backup but often Uninterruptible Power Supply (UPS) systems for zero-interruption power during transfer switches . Essential equipment includes surgical lights, anesthesia machines, and patient monitors.
Intensive Care Units: These areas support patients dependent on ventilators, infusion pumps, and continuous monitoring equipment. Power must be maintained without interruption.
Emergency Departments: As entry points for critical patients, these departments must function seamlessly during power outages.
Labor and Delivery Units: Similar to ICUs, these areas support vulnerable patients who may be dependent on electronic monitoring and life-support equipment.
For these critical areas, a comprehensive approach to hospital backup power requirements often involves both standby generators and UPS systems to bridge the gap until generators stabilize .
Generator Sizing and Capacity Calculations
Proper generator sizing is more important than simply counting units. An undersized generator can be as problematic as having no backup at all.
Load Bank Analysis: Conducting a detailed load analysis is the foundation of appropriate generator selection. This involves cataloging every device and system that requires backup power.
Starting Current Considerations: Equipment with motors (like HVAC systems) require significantly more power to start than to run. Generators must accommodate these surge currents without stalling.
Future Expansion: Generator capacity should include a margin (typically 15-25%) for future equipment additions and facility expansions.
Fuel Storage: Regulations often mandate minimum on-site fuel storage, typically 24-48 hours of continuous operation at full load, with provisions for emergency refueling .
The capacity calculations must reflect the actual demand of connected loads while considering growth and special electrical characteristics of medical equipment.
Integration with Other Backup Systems
Generators don't operate in isolation—they're part of a layered power protection strategy that addresses different types of power interruptions.
Uninterruptible Power Supply (UPS): UPS systems provide instantaneous battery-backed power for sensitive electronic equipment during the brief interval between utility failure and generator stabilization (typically 10-15 seconds) . They are essential for digital medical equipment and computer systems.
Automatic Transfer Switches (ATS): These critical components detect power failure and automatically switch to generator power. They must operate reliably and within the timeframes specified by codes.
Isolated Power Systems (IPS): In wet locations and certain critical care areas, isolated power systems enhance safety by limiting potential fault currents .
Redundant Power Feeds: Critical areas may require dual power feeds from separate generators to ensure redundancy at the distribution level.
This multi-layered approach creates a fault-tolerant system that maintains power quality and availability under virtually all circumstances.
Generator Quantity Configuration Scenarios
The number of generators varies based on hospital size, criticality, and budget considerations. Several common configurations address different levels of reliability needs.
Single Generator Configuration:
Suitable for smaller hospitals or critical access facilities
Must be sized to handle the entire emergency load
Carries risk of single point of failure
May be combined with UPS systems for critical areas
Multiple Generator Configuration (N+1 Redundancy):
The preferred approach for medium to large hospitals
Provides backup for the backup system
Allows for routine maintenance without compromising backup capability
May use multiple smaller units instead of one large generator
Dual Generator with Separate Systems:
Some facilities employ separate generators for life safety systems and equipment loads
Provides additional segregation of critical systems
May be required for tertiary care hospitals
The specific configuration should be determined through a risk assessment that considers the clinical consequences of power loss to various departments.
Compliance with Standards and Codes
Hospital backup power systems must comply with numerous international standards and codes that define minimum requirements for reliability and safety.
International Standards: Organizations like ISO (ISO 8528 series) provide guidelines for generator performance and design.
Medical Facility Standards: Documents like Health Technical Memorandum (HTM) 06-01 and ANSI/ASHRAE/ASHE Standard 170-2021 provide specific guidance for healthcare facilities .
National Electrical Codes: These typically define requirements for emergency power systems in healthcare facilities, including transfer time requirements.
Local Regulations: Municipal building codes often incorporate additional requirements specific to geographical risks like earthquakes, floods, or extreme weather.
Compliance with these standards represents the minimum threshold for hospital backup power requirements, with many institutions implementing systems that exceed these benchmarks.
Maintenance and Testing Protocols
A generator that isn't properly maintained is simply expensive ballast. Regular testing and maintenance are non-negotiable for ensuring reliability when needed.
Weekly Testing: Most codes require generators to be exercised under load on a regular basis to verify operational readiness.
Preventive Maintenance: Comprehensive maintenance programs include filter changes, fluid analysis, and inspection of critical components.
Load Bank Testing: Periodic testing with simulated loads verifies system performance under conditions mimicking actual power failure.
Fuel Quality Management: Diesel fuel requires active management to prevent degradation and microbial growth that can compromise generator operation.
Documentation: Proper records of all maintenance activities, tests, and repairs should be meticulously maintained as required by regulations .
These protocols ensure that when primary power fails, the backup system performs flawlessly regardless of duration or weather conditions.
Conclusion
Determining how many generators a hospital needs is a complex decision that balances regulatory requirements, clinical operations, and financial considerations. While a single generator may suffice for smaller facilities, larger hospitals typically require multiple units to ensure redundancy and adequate capacity for all critical systems. The most effective approach involves conducting a thorough load analysis, classifying areas by clinical criticality, and designing a system with appropriate redundancy. Ultimately, properly designed hospital backup power requirements are not just about compliance—they're about ensuring patient safety when the lights go out.
Our team specializes in helping healthcare facilities design and implement backup power solutions that meet their specific clinical needs and regulatory requirements. For a personalized assessment of your hospital's power needs, contact our experts at skala@whjlmech.com.